

 back to Dr. Reid's Corner Directory
back to Dr. Reid's Corner DirectoryFollow Up On The Sentinel Lymph Node Biopsy
 email this to a friend
email this to a friend
I have taken a few months off from writing the Lymphedema eNews articles. During this time I have reported the results of a clinical trial using a new treatment for patients with metastatic cancer of the colon. This trial uses a new form of gene therapy based on the common cold virus. While still early, the results of this trial is very encouraging (USA today article). The gene therapy technology is still in the early stages of development; however, I hope to someday be able to write that the promise of gene therapy has helped not only treat cancer, but helped to control and perhaps cure lymphedema. Until we reach that point, there is a lot of work to be done and we will continue our efforts to provide the most effective treatments for lymphedema.
In two issues of Lymphedema eNews, I have reported on the use of sentinel lymph node biopsy. A recent report raises an important question about when sentinel lymph node dissections can be safely used without risk of leaving behind lymph nodes involved with cancer. To help put the issue in perspective, I will summarize some of the discussion from my previous articles.
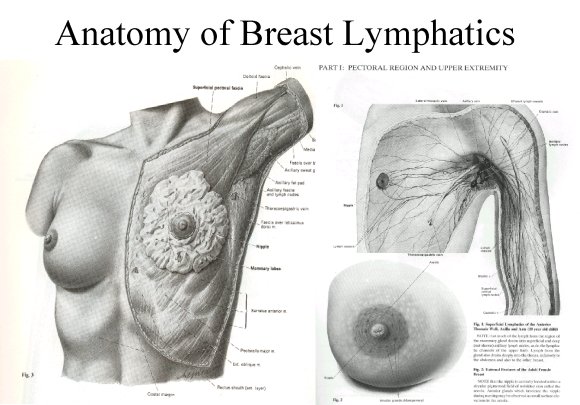
The status of the lymph nodes is the most important single prognostic factor for breast cancer. Cells from cancers of the breast will break off from the cancer and migrate through the lymphatic channels to the regional lymph nodes. As a result, removal of the lymph nodes serves two functions. First, the nodes can be studied under the microscope. If there are no cancer cells in the lymph nodes, the risk of recurrence of the cancer is much lower than if there is metastatic cancer in the lymph nodes and less aggressive treatment is required to control the cancer. Patients with cancer in their lymph nodes will require additional treatment and their chance of recurrence of the cancer is higher. Second, if the cancer does involve the lymph nodes, removal of as much of the cancer as possible is important to reduce the chance that the cancer will come back in the involved lymph nodes in the axilla.
In a traditional axillary dissection, a portion of the tissue in the axilla where the lymph nodes are found is removed. The lymph nodes are small structures, about the size of a small pea, located throughout the body. They serve as immunological filters to protect the body that primarily function to protect the body from infections. Cancer cells from the breast will migrate to the lymph nodes in the axilla where there are over 50 small lymph nodes. To determine whether there is cancer in the lymph nodes, a sample of 5 to 10 of these nodes are removed surgically and studied under the microscope. The risk is that as more lymph nodes are removed, the probability of developing lymphedema increases.
The sentinel lymph node biopsy is essentially minimal surgery. Instead of removing 5 to 10 nodes, the sentinel node biopsy removes the one lymph node most likely to have cancer cells. To do this, a new technique has been developed that uses a combination of a radioactive tracer and a color dye. The dye is injected around the tumor or into the biopsy cavity. The dye will migrate through the lymphatic channels to the regional lymph nodes drained by the cancer. The specific node most likely to be involved with cancer is then identified and removed for microscopic analysis.
In two issues of Lymphedema eNews, I have reported on the use of sentinel lymph node biopsy. A recent report raises an important question about when sentinel lymph node dissections can be safely used without risk of leaving behind lymph nodes involved with cancer. To help put the issue in perspective, I will summarize some of the discussion from my previous articles.
The status of the lymph nodes is the most important single prognostic factor for breast cancer. Cells from cancers of the breast will break off from the cancer and migrate through the lymphatic channels to the regional lymph nodes. As a result, removal of the lymph nodes serves two functions. First, the nodes can be studied under the microscope. If there are no cancer cells in the lymph nodes, the risk of recurrence of the cancer is much lower than if there is metastatic cancer in the lymph nodes and less aggressive treatment is required to control the cancer. Patients with cancer in their lymph nodes will require additional treatment and their chance of recurrence of the cancer is higher. Second, if the cancer does involve the lymph nodes, removal of as much of the cancer as possible is important to reduce the chance that the cancer will come back in the involved lymph nodes in the axilla.
In a traditional axillary dissection, a portion of the tissue in the axilla where the lymph nodes are found is removed. The lymph nodes are small structures, about the size of a small pea, located throughout the body. They serve as immunological filters to protect the body that primarily function to protect the body from infections. Cancer cells from the breast will migrate to the lymph nodes in the axilla where there are over 50 small lymph nodes. To determine whether there is cancer in the lymph nodes, a sample of 5 to 10 of these nodes are removed surgically and studied under the microscope. The risk is that as more lymph nodes are removed, the probability of developing lymphedema increases.
The sentinel lymph node biopsy is essentially minimal surgery. Instead of removing 5 to 10 nodes, the sentinel node biopsy removes the one lymph node most likely to have cancer cells. To do this, a new technique has been developed that uses a combination of a radioactive tracer and a color dye. The dye is injected around the tumor or into the biopsy cavity. The dye will migrate through the lymphatic channels to the regional lymph nodes drained by the cancer. The specific node most likely to be involved with cancer is then identified and removed for microscopic analysis.
The sentinel node technique removes fewer lymph nodes; however, there is a risk that residual cancer cells present in other lymph nodes may be left behind. The important question for the well being of the cancer patient is whether biopsy of one node is sufficient to insure that no cancer cells are missed. It would be a tragedy to allow a woman to die needlessly because an inadequate biopsy resulted in ineffective treatment.
Over the last 10 years improvements in mammography have resulted in the detection of breast tumors at earlier and earlier stages. The early detection of breast cancer means that the patients and their doctor must determine whether a sentinel node biopsy is adequate to determine the extent of cancer spread.
A recent study sought to identify the factors that favor the use of sentinel lymph node biopsy among patients who were detected with small tumors by routine mammography. In this study, Dr. Cutuli and colleagues analyzed the results of axillary dissection in 893 women who underwent lumpectomy and radiation for small tumors measuring about 1 inch or smaller. They found that about one quarter of the women with tumors measuring less than 1 inch had axillary lymph node involvement; however, they also found that most of the women with lymph node involvement had larger tumors and these tumors appeared more aggressive when studied under the microscope. These results are important since they suggest that the majority of women with small tumors detected on routine mammograms are good candidates for sentinel lymph node biopsy.
I recently presented data on the use of a new gene therapy treatment for patients with metastatic cancer involving the liver. While gene therapy holds the promise for the treatment of lymphedema in the future, I think we are making significant strides in the prevention of lymphedema. Routine mammograms are detecting breast cancer at earlier stages than ever before and current information suggests that the majority of these women can safely undergo sentinel lymph node biopsy.
Sincerely,
Tony Reid MD Ph.D
Cutuli B, Velten M, Martin C. Assessment of axillary lymph node involvement in small breast cancer: analysis of 893 cases. Clin Breast Cancer 2001 2:59-65
Over the last 10 years improvements in mammography have resulted in the detection of breast tumors at earlier and earlier stages. The early detection of breast cancer means that the patients and their doctor must determine whether a sentinel node biopsy is adequate to determine the extent of cancer spread.
A recent study sought to identify the factors that favor the use of sentinel lymph node biopsy among patients who were detected with small tumors by routine mammography. In this study, Dr. Cutuli and colleagues analyzed the results of axillary dissection in 893 women who underwent lumpectomy and radiation for small tumors measuring about 1 inch or smaller. They found that about one quarter of the women with tumors measuring less than 1 inch had axillary lymph node involvement; however, they also found that most of the women with lymph node involvement had larger tumors and these tumors appeared more aggressive when studied under the microscope. These results are important since they suggest that the majority of women with small tumors detected on routine mammograms are good candidates for sentinel lymph node biopsy.
I recently presented data on the use of a new gene therapy treatment for patients with metastatic cancer involving the liver. While gene therapy holds the promise for the treatment of lymphedema in the future, I think we are making significant strides in the prevention of lymphedema. Routine mammograms are detecting breast cancer at earlier stages than ever before and current information suggests that the majority of these women can safely undergo sentinel lymph node biopsy.
Sincerely,
Tony Reid MD Ph.D
Cutuli B, Velten M, Martin C. Assessment of axillary lymph node involvement in small breast cancer: analysis of 893 cases. Clin Breast Cancer 2001 2:59-65
Dr. Reid's Corner